Use Your Head: Understanding the Unseen Effects of Concussions
by Abigail Smith
December 2022
A slip on the winter ice causes a neighbor to smack their head. A high school athlete takes a tough blow during a competitive game. A car accident leaves passengers with bruising on their foreheads from the impact. Although these injuries are often dismissed as a simple bump on the head, they illustrate some of the most common causes of traumatic brain injuries.
A traumatic brain injury caused by a bump, blow, or jolt to the head – or even the entire body – results in disruption of normal brain function. Commonly known as a concussion, the brain disruption caused by a mild traumatic brain injury is similar to an earthquake's disruption of a highway. Just as an earthquake can shake up a highway impairing travel by car, a brain injury damages brain cells and disrupts the communication circuits throughout the brain. In turn, these brain changes drive many symptoms experienced by individuals following a concussion.
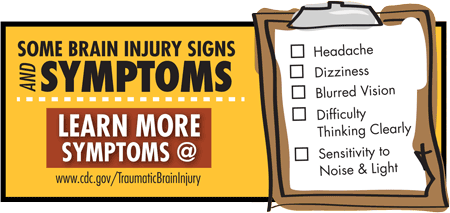 It
is important to recognize that traumatic brain injuries
are often invisible, meaning that someone may not have
cuts, bruising, bleeding, or other visible signs of
injury. Despite the lack of blood and bruises, a blow to
the head can cause forgetfulness, mental fogginess,
difficulty concentrating, changes to sleep, headaches,
dizziness, visual changes, nausea, irritability, and mood
changes. Danger signs include unresponsiveness, one pupil
larger than the other, worsening headache, repeated
vomiting, slurred speech, weakness, numbness, or
decreased coordination. Presence of any of the danger
signs following a hit to the head warrants immediate
evaluation by a medical professional.
It
is important to recognize that traumatic brain injuries
are often invisible, meaning that someone may not have
cuts, bruising, bleeding, or other visible signs of
injury. Despite the lack of blood and bruises, a blow to
the head can cause forgetfulness, mental fogginess,
difficulty concentrating, changes to sleep, headaches,
dizziness, visual changes, nausea, irritability, and mood
changes. Danger signs include unresponsiveness, one pupil
larger than the other, worsening headache, repeated
vomiting, slurred speech, weakness, numbness, or
decreased coordination. Presence of any of the danger
signs following a hit to the head warrants immediate
evaluation by a medical professional.
According to the Minnesota Department of Health, brain injuries are very common with around 10,000 Minnesotans sustaining a traumatic brain injury every year. In Big Stone County and surrounding areas, 15- to 19-year-olds represent the majority of individuals presenting to emergency rooms with traumatic brain injuries. Experts link the injury rate with this age group's adolescent activities, including participation in competitive sports, inexperience as new motor vehicle drivers, and age-related testing of life's boundaries.
Moving attention from injury causes to recovery efforts, these same age-related factors provide challenges for teachers, coaches, parents, and teenagers themselves. With ongoing brain development at this age, a concussion can cause learning difficulties, often first noticed by teachers. For these students, school officials may recommend individualized academic accommodations. Coaches may insist a teen sit out from sports because they know a second injury following a concussion can have devastating long-term consequences. Parents often notice increased irritability, sadness, or mood changes in their children. Teens may find life after a concussion frustrating with new challenges at school and temporary sport restrictions. Despite frustrations, recovery efforts must be upheld to allow teens' brains time to heal and get them back to learning, athletics, and normal routines.
 Although teenagers make up a majority of concussions, no
one is risk-free from a brain injury. Members of all age
groups must familiarize themselves with protection and
prevention strategies. Strategies range from always
buckling a seatbelt to wearing a helmet when riding
anything that moves at high speeds. Children should be
secured into vehicles with proper car seats. Older adults
should remove rugs that catch their feet and ensure their
vision is clear enough to see obstacles. Seniors also
benefit from strength and balance exercises to prevent
falls.
Although teenagers make up a majority of concussions, no
one is risk-free from a brain injury. Members of all age
groups must familiarize themselves with protection and
prevention strategies. Strategies range from always
buckling a seatbelt to wearing a helmet when riding
anything that moves at high speeds. Children should be
secured into vehicles with proper car seats. Older adults
should remove rugs that catch their feet and ensure their
vision is clear enough to see obstacles. Seniors also
benefit from strength and balance exercises to prevent
falls.
However, despite preventative efforts, accidents and traumatic brain injuries can still occur. Local resources to help manage the immediate and long-term effects of a traumatic brain injury include local emergency services, doctors, other medical professionals, and even state-wide support groups.
Knowing and recognizing the brain injury danger signs can be lifesaving. It is just as important to understand this: When someone hits their head, no mark does not mean there is no brain injury.
This article also appeared in the December 13, 2022 issue of the Ortonville Independent.
About the Author
 Abigail Smith is a third-year medical student at
the University of North Dakota School of Medicine &
Health Sciences. She was selected as the Ortonville
participant for the school's ROME program, or Rural
Opportunities in Medical Education. Because the program
includes teaching student doctors about the importance of
how rural newspapers can deliver health information, she
has written this column for her ROME community. The
information is not for diagnosis or treatment and should
not be used in place of previous medical advice provided
by a licensed practitioner.
Abigail Smith is a third-year medical student at
the University of North Dakota School of Medicine &
Health Sciences. She was selected as the Ortonville
participant for the school's ROME program, or Rural
Opportunities in Medical Education. Because the program
includes teaching student doctors about the importance of
how rural newspapers can deliver health information, she
has written this column for her ROME community. The
information is not for diagnosis or treatment and should
not be used in place of previous medical advice provided
by a licensed practitioner.
